

1. Case Summary
Female, 24 years old
History: Underwent right frontotemporal craniotomy for craniopharyngioma resection 2 years agoChief complaint: Progressive vision loss for 3 months
Visual acuity: Right eye 0.08, left eye: counting fingers at 20 cm
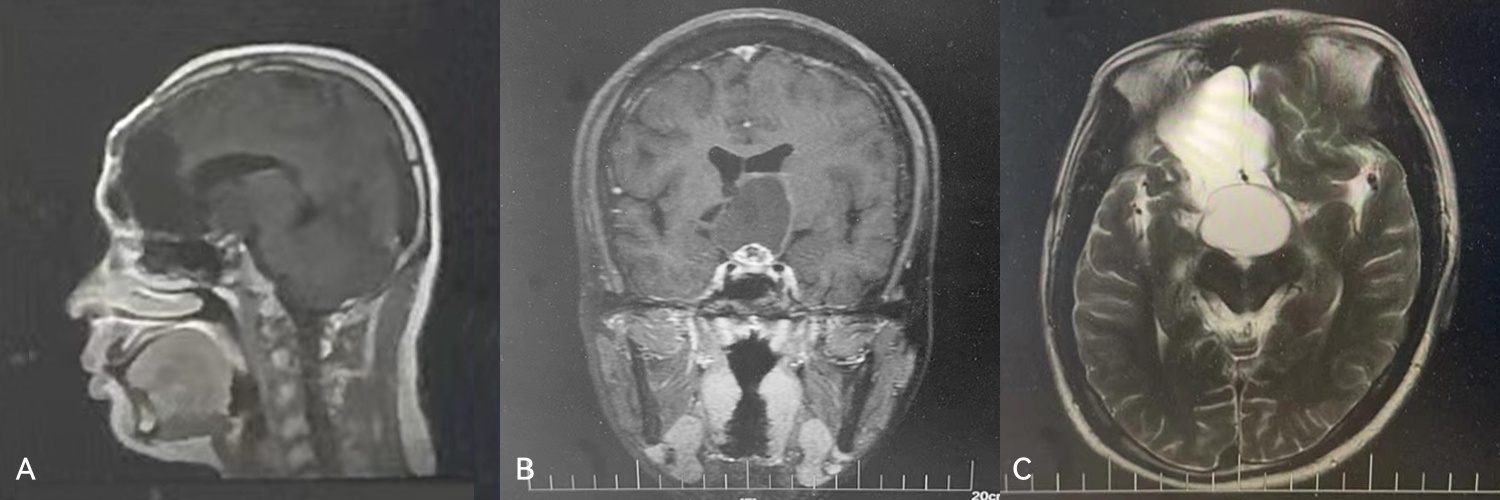
MRI Findings: Postoperative changes following right frontotemporal craniotomy for craniopharyngioma; right frontal encephalomalacia; suprasellar cystic-solid lesion(Figure 1A-1C)
Diagnosis: Recurrent craniopharyngioma
2. Treatment Plan and Surgical Procedures
Intraoperative Technique:
The tumor was completely resected through the pituitary–optic chiasm corridor, with opening of the third ventricle.
Skull Base Reconstruction Strategy:
Subdural placement of autologous fat to fill the large surgical cavity and buffer cerebrospinal fluid (CSF) pulsation
Subdural placement of artificial dura mater to form a temporary watertight seal
Epidural placement of fascia lata to close the dural defect
A pedicled nasoseptal mucosal flap was placed over the fascia lata to provide vascular supply and promote scarring and healing of the skull base
Dural sealant was applied over the mucosal flap to secure it and create a watertight environment to prevent CSF leakage
Surgical procedures:
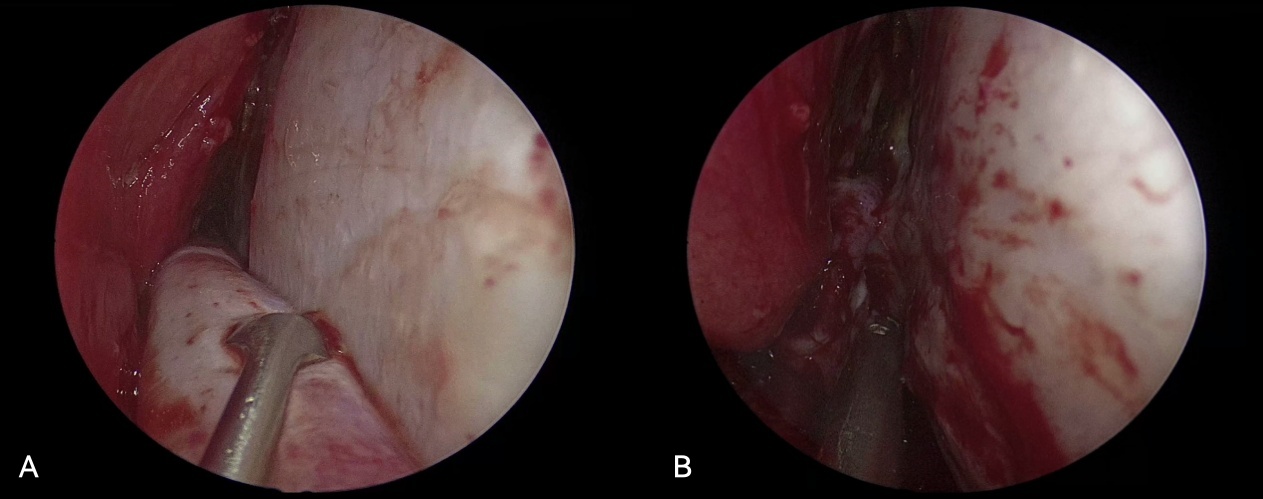
FIGURE 2:(A-B)Harvesting of the Pedicled Nasoseptal Flap
A
vascularized pedicled nasoseptal mucosal flap is raised to provide
blood supply to the subsequent fascia lata layer during skull base
reconstruction.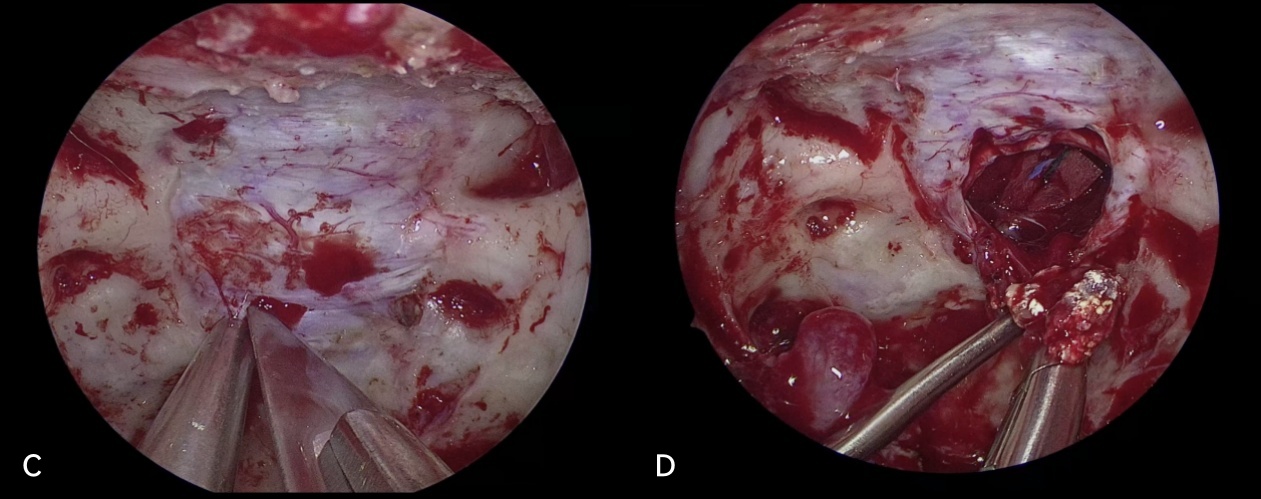
FIGURE
3:(C-D)Gross Total Resection (GTR) of the Tumor via the Pituitary–Optic
Chiasm Corridor and Opening of the Third Ventricle
(C). Dural incision at the sellar floor
(D). Gross total resection of the tumor through the pituitary–optic chiasm corridor
Skull Base Reconstruction Procedures-
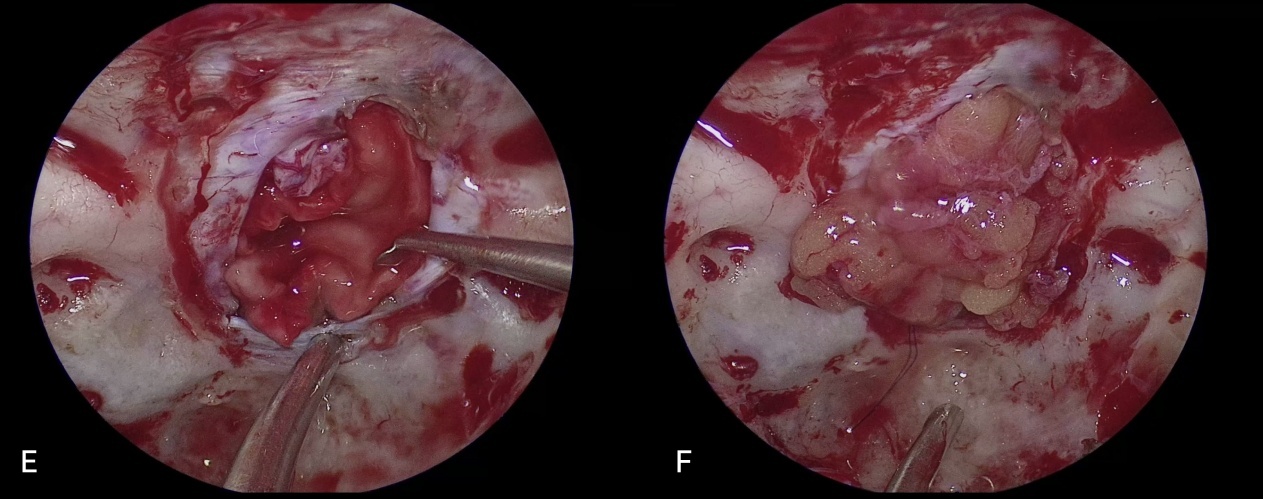
FIGURE 4:(E)Placement of an Absorbable, Watertight Dural Substitute
Temporarily seals the defect in a watertight manner and promotes.
FIGURE 5:(F) Subdural Placement of Autologous Subcutaneous Fat
Fills large surgical defects and buffers pressure pulsation from cerebrospinal fluid (CSF).
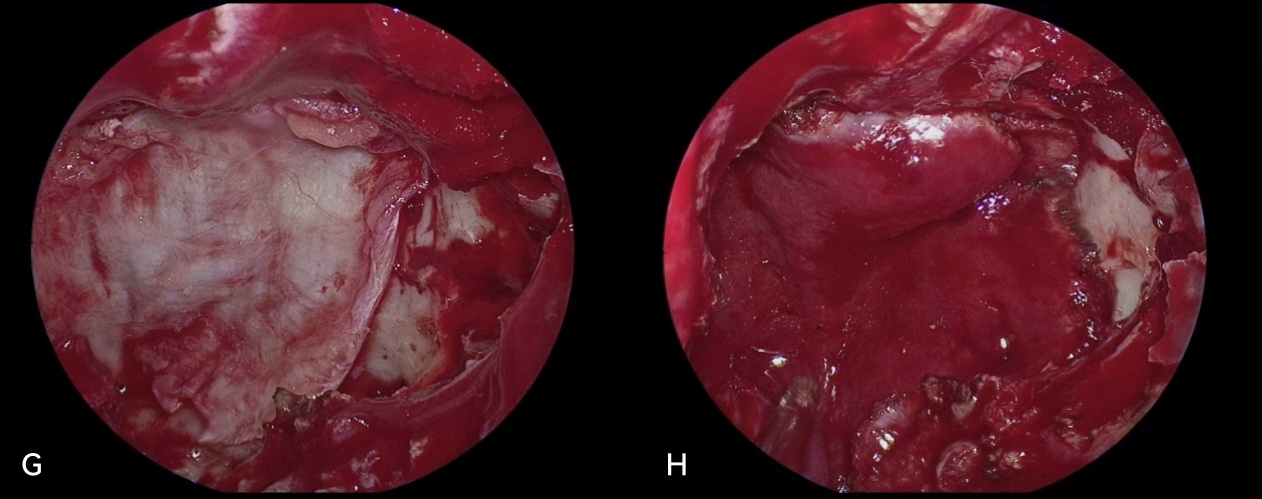
FIGURE 6:(G)Epidural Placement of Fascia Lata
Provides external reinforcement to seal the dural defect.
FIGURE 7:(H)Overlay of the Vascularized Pedicled Nasoseptal Flap on the Fascia Lata
Supplies vascularization to the fascia lata, enhancing healing and scar
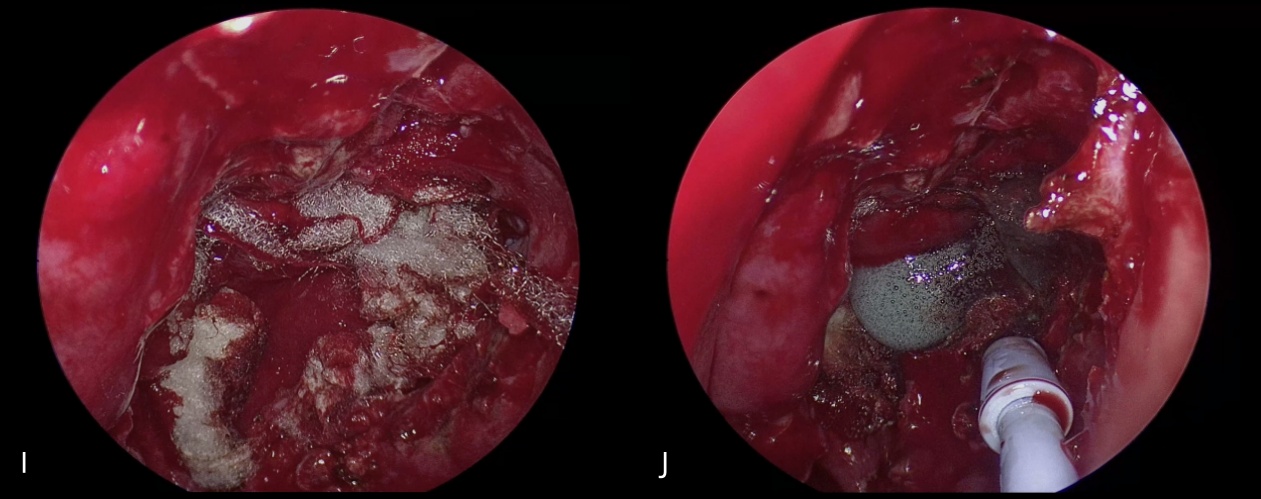
FIGURE 8:
(I)Application of Oxidized Regenerated Cellulose(ORC) on the Outer Surface of the Nasoseptal Flap
Aids faster hemostasis and reduced
(J)Spraying of Absorbable PEG-based Dural Sealant over the Nasoseptal Flap
Creating a watertight environment to prevent CSF leakage.
3. Postoperative Outcome
The patient recovered well after surgery
Visual acuity improved to 0.5 in the right eye and 0.3 in the left eye
No cerebrospinal fluid rhinorrhea was observed
4. Case Discussion / Reflections
Purpose of Skull Base Reconstruction:
To convert an open surgical cavity into a sealed environment, preventing CSF leakage and infectionPrinciples of Skull Base Reconstruction:
Multilayer composite repair to serve as both a physical barrier and biological scaffold for tissue regenerationKey Points of Reconstruction:
Ensuring vascular supply and eliminating dead spacePersonalized selection of materials and methods based on defect characteristics
———————————————————————————————————————————————
Chinese Expert Consensus on Skull Base Reconstruction Techniques in Endoscopic Endonasal Skull Base Surgery
I. Multilayer Composite Skull Base Reconstruction Using Free Tissue
(1) Standard Repair (Kelly Grade 0)
Indications: Intact dura/arachnoid during surgery, with no visible CSF leak
Steps:
Achieve hemostasis in the tumor cavity
Cover with absorbable artificial dura
Apply dural sealant or biological glue around the periphery
Place gelatin sponge
Nasal cavity is packed with expandable absorbable hemostatic material
(2) Multilayer Composite Reconstruction (Kelly Grade 1–2)
Indications: Arachnoid defect < 1 cm
Steps:
Place absorbable artificial dura under the dural defect
Insert autologous fat subdurally
For the epidural layer, use autologous fascia lata / free nasal mucosa / dural sealant / biological glue / muscle fascia to seal the defect margins
Apply a thin outermost layer of gelatin sponge or oxidized regenerated cellulose
Use balloon, gauze, or other spacers for support
II. Vascularized Flap–Based Skull Base Reconstruction (Kelly Grade 3)
Indications: Dural or arachnoid defects ≥1 cm, or high-flow CSF leaks due to exposure of the ventricles or basal cisterns
Steps:
Perform tumor resection and cavity hemostasis
For small defects, autologous fat may be sufficient
For large defects where fat is difficult to secure, place absorbable artificial dura or muscle fascia subdurally
Use dural sealant or biological glue to close gaps and secure the nasoseptal mucosal flap
Cover the flap with gelatin sponge
Place expandable sponge, iodoform gauze, or an inflated Foley balloon at the outermost layer to support the reconstruction materials
III. Suturing-Based Skull Base Dural Reconstruction
Indications: Large-area defects or repeated repairs
Approach:
Suturing
absorbable artificial dura / muscle fascia / nasal mucosa / pedicled
tissue flaps directly to the native skull base dura
Reference:
Hong
Tao, Zhang Yazhuo, et al. Expert Consensus on Skull Base Reconstruction
Techniques in Endoscopic Endonasal Skull Base Surgery. Chinese Journal
of Neurosurgery, November 2020, Vol. 36, No. 11.
———————————————————————————————————————————————
Author Biography
Li Chuzhong
Chief Neurosurgeon
Doctoral Supervisor
Deputy Director of Neuro-Oncology Ward III, Beijing Tiantan Hospital
Vice Chairman, Translational Medicine Branch, Chinese Society of Gerontology and Geriatrics
Standing Committee Member, Neurorestoration Committee, Chinese Medical Doctor Association
Standing Committee Member, Neuro-Oncology Branch, Chinese Neuroscience Society
Dr.
Li has conducted extensive work in endoscopic treatment of skull base
tumors such as pituitary adenomas, craniopharyngiomas, and chordomas, as
well as intraventricular disorders. Internationally, he was the first
to identify the SF3B1R625H hotspot mutation in prolactinomas, advancing
the understanding of pituitary tumor pathogenesis.
He
has authored over 40 SCI-indexed publications as first or corresponding
author, published one academic monograph, led six
national/provincial-level research projects, and holds 15 invention
patents and 4 software copyrights.
He
was selected for the Beijing Outstanding Young Talent Support Program
in 2015 and received the "Wang Zhongcheng Neurosurgery Young Physician
Award" in 2021.






